The Next Big Thing in Regenerative Medicine and PRP Therapy
Introduction to PRP Therapy
Over the last 10 years or so, platelet-rich plasma (PRP) and PRP therapy have gained greater recognition amongst the medical community, and for good reason. Famous Athletes, including Tiger Woods and Raphael Nadal, have used it to speed up recovery and improve the healing of various musculoskeletal injuries. Other individuals, like Kim Kardashian, have popularized it for its anti-aging effects through a cosmetic treatment coined “The Vampire Facial”.
Traditionally speaking, PRP therapy has been used in Orthopedics for intra-articular injections. It has been known to treat more chronic conditions, such as arthritis, as well as acute sports injuries including a torn meniscus, tendinopathies, muscle injuries, and more. However, it is now being explored through other routes of administration and producing incredible results.
PRP therapy is now being given intravenously to treat more systemic health conditions. Patients suffering from neurological diseases including Parkinson’s, Multiple Sclerosis, and Cerebral Palsy, are seeing positive results with autologous platelets given IV. Other conditions such as Lupus, Rheumatoid Arthritis, and Chronic Fatigue have also shown remarkable improvement.
While PRP therapy has notoriously produced inconsistent results, we discovered the next big thing in PRP that eliminates inconsistencies: TruDose PRP. This is a personalized treatment and, when given intravenously, generates clinical results that speak for themselves.
For those of you out there who are interested in regenerative medicine, such as stem cell therapy, keep reading…
So, What is Platelet-Rich Plasma Therapy?
Your blood is made up of several constituents. The majority of whole blood consists of a light, yellow liquid known as plasma. It also contains three other main components that flow within the plasma: platelets, red blood cells, and white blood cells. In the most simplistic terms, PRP is plasma with a high concentration of platelets.
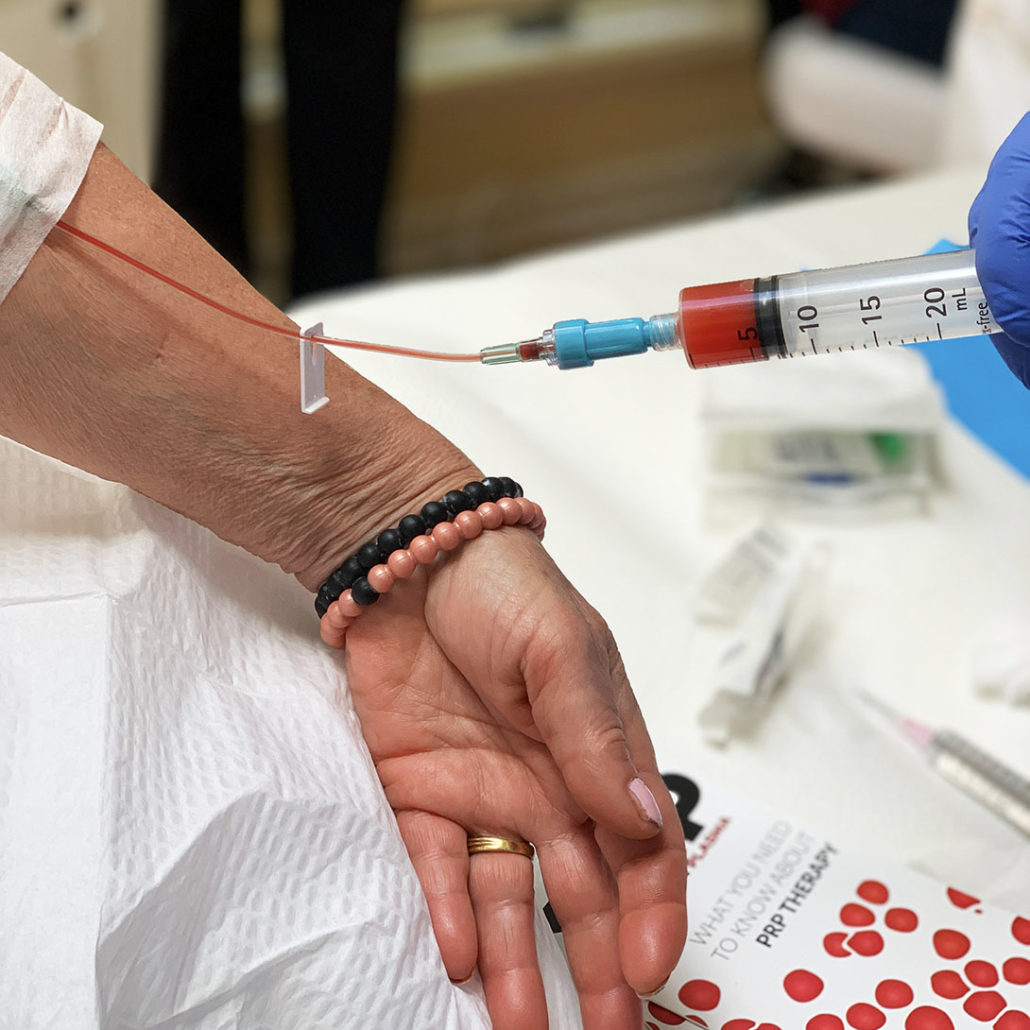
In order to obtain PRP, whole blood is drawn from the patient and spun in a centrifuge. Due to the different specific gravities of each blood component, platelets can be separated from red and white blood cells through centrifugation. After adequate separation has been achieved, the remaining plasma with a high concentration of platelets is drawn up and injected into the same patient.
What are the Benefits of PRP Therapy and What Can it Treat?
“We’re way past knee pain. I’m way past making my hair grow. We’re onto things that are unlocking and unlayering these real problem conditions.”
Tapley Holland, Bridging Biosciences
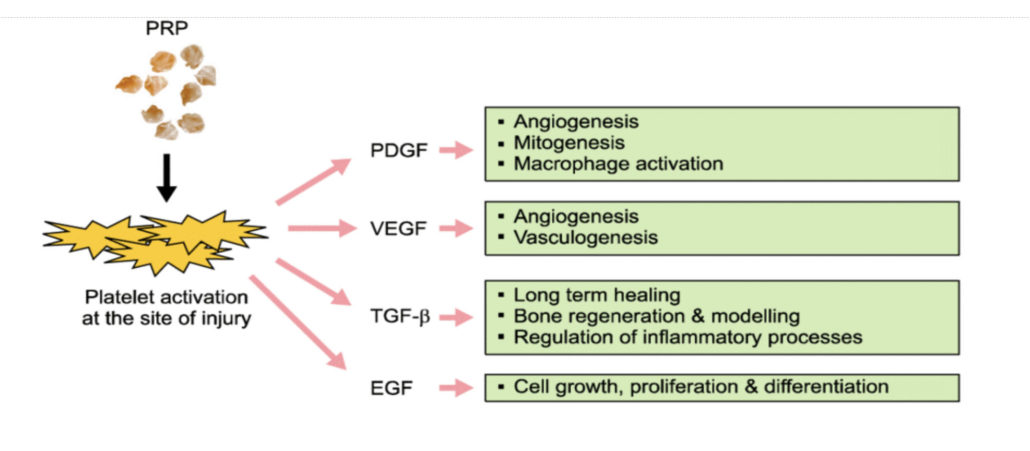
Most people associate platelets with their role in coagulation, especially in acute settings such as a laceration. While it’s true that they are prodigious in hemostasis, we are now discovering that their benefits extend far beyond simplistic wound healing. As it turns out, platelets are multi-functional key players in the modulation of angiogenesis, regeneration of tissue (recruiting stem cells), as well as innate and adaptive immune responses. This means that they are monumentally more essential to our immune systems as well tissue modulation and reorganization than we originally thought. You can think of platelets as circulating, paramedic drones. They survey our bodies, recognize immediate threats (whether it be a damaged blood vessel, damaged tissue, a microbe, etc.) and send signals for help while simultaneously providing acute support.
Harvesting these benefits from platelets in a clinical setting is now possible through platelet-rich plasma therapy. The body recognizes a higher dose of platelets (in comparison with the other components of blood), and immediately puts them to work. When given as a local injection, the PRP is allowed to work on that particular area alone. However, when given intravenously, a more systemic healing effect is achieved. Due to this, PRP therapy can be used to treat a whole host of diseases, including autoimmune diseases. Practitioners across the United States utilizing intravenous TruDose PRP therapy have seen dramatic improvements in patients with the following diseases:
- Rheumatoid Arthritis
- Lupus
- Hashimoto’s Thyroiditis
- Lyme Disease
- Parkinson’s Disease
- Multiple Sclerosis
While IV PRP therapy is particularly beneficial for neurological diseases and autoimmune-type conditions, it can treat a whole host of medical problems. It is, in its essence, anti-aging and beneficial for just about everyone.
How Does PRP Therapy Work?
PRP Therapy falls under the category of “Regenerative Medicine.” The platelets within PRP contain a number of growth factors (such as TGF, PDGF, IGF, and VEGF) that stimulate a healing response. They have the ability to repair damaged tissue, whether it be chronic or acute, and help the body fight off infection through their antimicrobial benefits. As you can see, they possess great clinical potential. Despite this fact, the results of PRP therapy have been inconsistent amongst patients. Some patients do well, while others see no improvements. Thankfully, we’ve found a solution to this remedial deficit by guaranteeing that each patient is given a therapeutic dose: TruDose PRP.
Why is TruDose PRP Therapy the Next Big Thing in Medicine? The Devil is in the Dosage.
“If a tissue is injured, does it really require a critical number of cells that actually start the healing process? The answer is yes. And is there a critical number of cells that could actually lead to inhibitory things? The answer is yes. And so, if you look at PRP in general, I’m just going to say probably 98% of what is being done across America, aesthetic based and sports medicine based, is not even scratching the surface to what a therapeutic dose should be.”
Tapley Holland, Bridging Biosciences
Like with all treatments and medication, the key to achieving clinical efficacy is simple: you need the appropriate dose. In order to reach any type of therapeutic benefit, platelets must be at a concentration of 1.5 billion platelets per milliliter. Since every patient is different and has varying platelet levels, each will require different amounts of blood to be withdrawn and spun down through centrifugation.
TruDose PRP was created to solve this variability. Utilizing artificial intelligence to analyze your blood, it can compute the exact amount of blood each patient needs to have drawn in order to achieve a therapeutic dose. This has generated consistent, patient-specific treatments with excellent outcomes.
Why IV Instead of Localized Injections?
Intravenous PRP therapy allows the body, in its innate wisdom, to direct it towards areas of degeneration. For example, IV PRP can lead to the regeneration of the central nervous system if that area is damaged. This is similar in the ways that IV stem cells work. Nonetheless, we believe that intravenous autologous PRP is potentially better than stem cell therapy and here’s why:
- It recruits your very own stem cells instead of using donor cells.
- It lays the foundation for stem cells to regenerate tissue. For tissue to truly regrow, it needs some basic “soil”. There has to be a certain degree of inflammation, followed by granulation and angiogenesis. Once these are in place, stem cells come in during re-epithelialization and tissue remodeling to work their full magic. If you miss one of these steps, the results will be less satisfactory. Platelet-rich plasma has the benefit of creating good soil for stem cells to reach their full potential.
- It is more affordable. Intravenous stem cells can cost anywhere from $5,000-20,000 while IV PRP costs around $3,500.
Is TruDose PRP Therapy Safe?
Since PRP therapy uses autologous blood (withdrawn from the patient and given back to the same patient), it is incredibly safe. No additives are placed within the PRP before it is returned to the patient. So far, no adverse reactions have been seen with IV PRP therapy. The only risk noted has been a potential, small skin infection from the venipuncture. According to the TruDose creator, Tapley Holland, there have not been any increased risks of clotting noted with IV PRP therapy. Patients with a higher risk of thrombosis (including cancer, blood-clotting disorders, etc.) have also been treated without issue.

Is TruDose the Future of Regenerative Medicine?
The future of regenerative medicine lies in scientifically-based methods of practice that facilitate the body’s own repair mechanisms to heal itself. TruDose PRP therapy falls under this category. We believe that its combination of artificial intelligence with safe, scientifically proven PRP therapy will allow us to eliminate inconsistencies and reach new levels of healing. At the end of the day, each patient’s own body is beautifully designed to repair itself. As practitioners, our job is to support our patients and give their bodies the information and tools they need in order to heal. Staying true to our commitment to Innovative Medicine, we are excited to implement TruDose PRP into our practice and anticipate having outstanding results.
As always, we’re devoted to uncovering synergistic treatments that can amplify positive outcomes. Be sure to keep following along with us as we research and share the ways that we can further improve Trudose PRP.
The post The Next Big Thing in Regenerative Medicine and PRP Therapy appeared first on Innovative Medicine.
See how we can help you restore complete health of body, mind & spirit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et